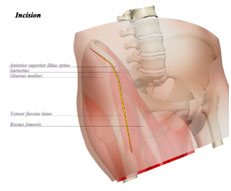
Hip replacement surgery is one of the most successful procedures in medicine. While there are several approaches to enter the hip joint to remove arthritic cartilage and diseased bone, there are primarily two approaches that involve minimal trauma to the hip abductors—muscles that are critical for a normal walk and speedy recover. These two approaches are the anterior approach (through the front of the hip) and the mini-posterior (just behind the top of the femur). While there are some subtle differences between the approaches, the most important factor in a successful hip replacement is restoring normal anatomy (leg length, hip center, offset) with well-positioned components.
Muscles are split or moved in anterior hip and mini posterior. Neither approach involves removal or partial resection of any muscle. The anterior approach utilizes an internervous plane while the mini-posterior involves splitting the gluteus maximus.

| Anterior Approach | Minimally Invasive Posterior Approach |
| Increased risk to lateral femoral cutaneous nerve (nerve to the front of the thigh) |
Minimal risk to large skin nerves |
| Scar visible in the front of the hip | Scar just behind femur that is difficult to see |
| Higher likelihood of anterior dislocation1 | Higher likelihood of posterior dislocation1 |
| Hospital stay around 2.0 days | Hospital stay around 2.3 days |
| Ambulation with no assist at 7-24 days2 | Ambulation with no assist at 10-30 days |
| Increased use of x-rays3 | No routine usage of x-rays |
| Complication rates increase with higher BMI patients | Less complications in higher BMI patients |
1. The dislocation rates for both approaches, in experienced hands, is around 0.6% for the diagnosis of osteoarthritis.
2. Low level studies that show some early benefit with anterior hip replacement typically compare healthy, active patients to higher BMI, more sedentary patients. Thus, the differences have little to do with the approach.
3. Fluoroscopy is routinely used for cup placement which increases radiation to the genitalia.
